Subscribe to Pittwire Today
Get the most interesting and important stories from the University of Pittsburgh.Targeting Immune Cells that Help Tumors Stay Hidden Could Improve Cancer Immunotherapy
Researchers at the University of Pittsburgh School of Medicine and UPMC have discovered a clue about how to improve the success of immunotherapy drugs to successfully treat more cancers.
Immunotherapy drugs push the immune system itself to detect and kill cancer cells, and they have been successful against several types of aggressive cancers, including some melanomas and lung cancers. However, these drugs are only effective in some 10 to 30 percent of patients with certain tumor types. Exactly why these drugs don’t work in more patients has remained a mystery.
The Pitt/UPMC discovery, published in Cell, points to what could be an important mechanism by which current immunotherapy drugs work. Learning more about this mechanism might give researchers a new approach to making the drugs more effective.
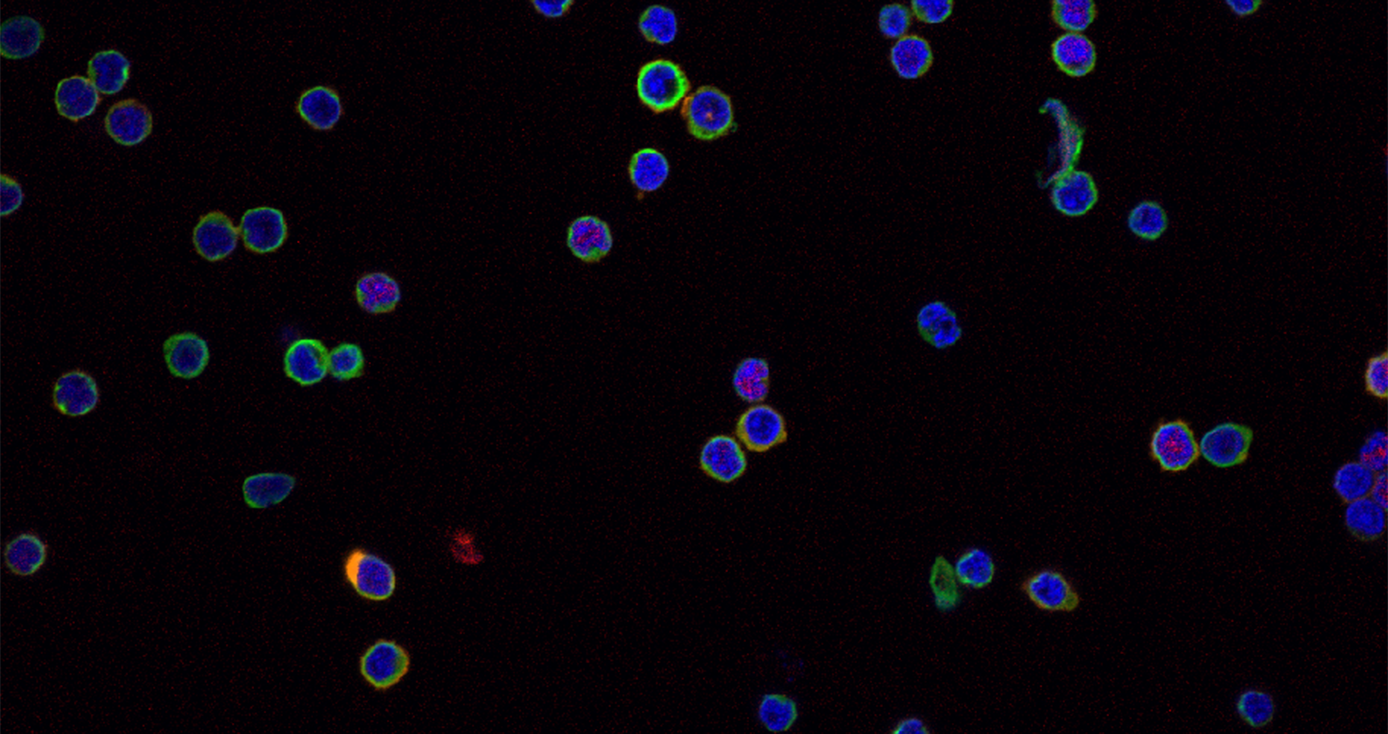
Their findings showed that targeting a subpopulation of immune cells called regulatory T cells could be an effective approach to treating cancers. Regulatory T cells (Tregs, pronounced “tee-regs”) help maintain a delicate balance in the immune system.
“They act like a dimmer switch, keeping the lights bright enough to detect and eliminate threats, but not so bright that our own cells are hurt,” said Dario Vignali, who holds the Frank Dixon Chair in Cancer Immunology, and is professor and vice chair of immunology at Pitt’s School of Medicine.
“In cancer, Tregs can be detrimental because by turning down the lights, they prevent the immune system from detecting and killing cancer cells. While creating drugs to eliminate Tregs may seem like a logical approach to treatment, they could lead to life-threatening autoimmune complications, making them unusable in cancer patients. Thus, we need to identify approaches that selectively target Tregs in tumors, sparing those outside the tumor,” said Vignali, who also is co-director of the Cancer Immunology Program at the UPMC Hillman Cancer Center.
Building toward the discovery
The basis for this new discovery began a few years ago, when Vignali and his colleagues discovered that a surface protein called neuropilin-1 (Nrp1) was required to maintain the function, integrity and survival of Tregs within the harsh tumor microenvironment.
Importantly, blocking or deleting the Tregs’ Nrp1 in mice only impacted their function in tumors — not in the rest of the body — resulting in tumor eradication without inducing autoimmune or inflammatory disease.
In the current study, Vignali's team confirmed that Nrp1 had been preventing the immune system from beating the tumor. When Tregs lose the protein, "they become active participants in the anti-tumor immune response,” said Vignali. To see if the findings could apply to humans, they also looked at the protein's expression in cancer patients with poor prognoses. These patients' Tregs indeed expressed more of the protein.
To arrive at their findings, the researchers created a genetically modified mouse model in which the Nrp1 gene was deleted in half the Treg cell population, but not the other half. Tumor growth in this model, they found, was dramatically reduced when compared to a normal mouse in which Nrp1 was present in all Tregs.
In other words, the Tregs without Nrp1 couldn't turn down the lights to hide the cancer.
“This allowed the immune system to see and attack the tumor,” said Abigail E. Overacre-Delgoffe, a graduate student in Vignali’s lab and the first author of the Cell study. Those Tregs also couldn't block their normal counterparts outside the tumor from performing their immunosuppressive functions. Genomic and cellular analyses revealed that a secreted immune molecule prevented the dimmer switch function of Tregs in the mice, particularly and selectively in the tumor microenvironment.
Vignali says the molecule, called interferon-gamma, “seems to make Tregs fragile so that they lose their suppressive function, but only in the tumor. Thus, maybe making Tregs fragile is a critical requirement for effective immunotherapy.”
Future implications
Overall, the authors note that their findings are significant because they show that if we can get a portion of the tumor-associated Tregs to lose their immunosuppressive functions — possibly by using interferon-gamma — it may be enough to set off a chain reaction where those cells could influence other tumor-associated Tregs, consequently promoting anti-tumor immunity without inducing autoimmune conditions as a side effect. Additionally, in the near-term, tracking Treg functional fragility may prove to be an effective approach to monitor whether immunotherapy treatments are effective in patients.